First of all,
Pediatric neurology, particularly in the context of epilepsy, necessitates a sophisticated and specialized approach. Epilepsy, a neurological illness marked by recurring seizures, manifests differently in children compared to adults. Understanding the particular characteristics of juvenile epilepsy is critical for providing effective therapy and improving outcomes for young patients. In this essay, we delve into the intricacies of epilepsy in children and discuss the particular care necessary in pediatric neurology.
Understanding Pediatric Epilepsy:
Epilepsy is one of the most frequent neurological illnesses affecting children, with varied origins and presentations. Unlike adults, children with epilepsy often face various seizure types and developmental issues. The etiology of pediatric epilepsy includes a wide spectrum, including genetic causes, brain abnormalities, prenatal traumas, infections, and metabolic diseases.
Seizure presentation in children can be variable, ranging from modest episodes like staring spells or brief lapses in awareness to more violent convulsions. Moreover, seizures may interfere with critical developmental milestones, altering cognitive, behavioral, and social elements of a child's life. Recognizing and diagnosing epilepsy in children needs a multidisciplinary approach, comprising pediatric neurologists, epileptologists, neuropsychologists, and other allied healthcare experts.
Challenges in Diagnosis and Management:
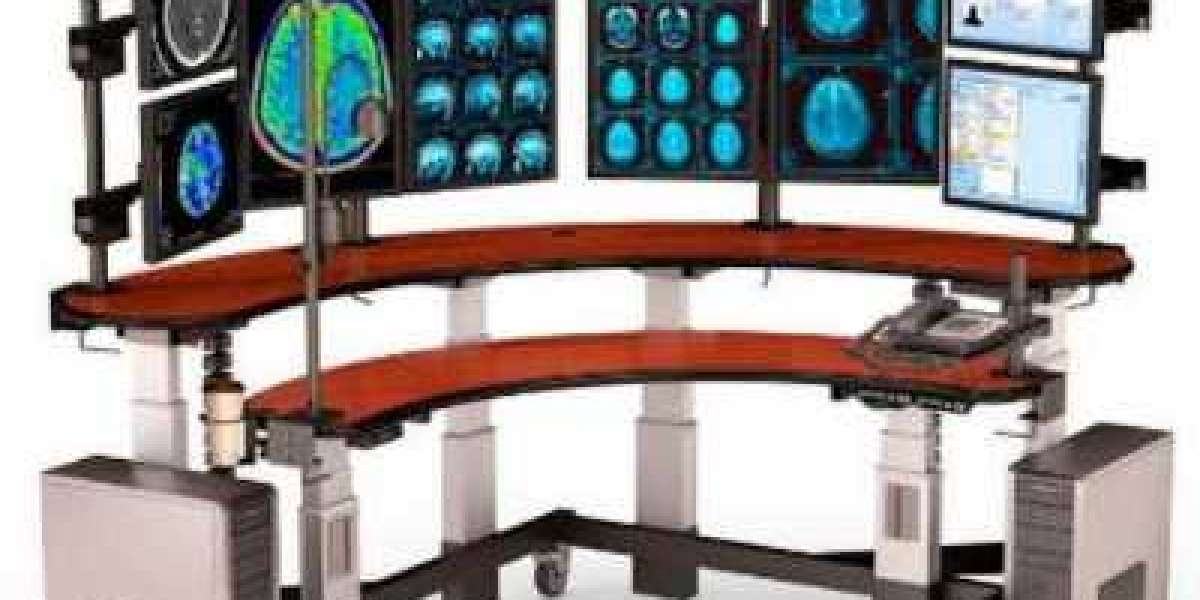
Diagnosing epilepsy in children involves distinct challenges due to their ongoing brain development and limited capacity to describe symptoms. Moreover, separating epileptic seizures from other paroxysmal occurrences, such as breath-holding spells or syncope, requires careful clinical evaluation and diagnostic testing. Advanced neuroimaging techniques, including magnetic resonance imaging (MRI) and electroencephalography (EEG), play a vital role in identifying underlying structural abnormalities and epileptiform activity in the brain.
Once identified, the therapy of pediatric epilepsy requires a personalized approach, including criteria such seizure type, frequency, related comorbidities, and developmental needs. While antiepileptic drugs form the cornerstone of treatment, establishing seizure control typically demands a balance between efficacy and potential unwanted effects. Furthermore, non-pharmacological therapies like ketogenic diet therapy, epilepsy surgery, and neuromodulation techniques offer other paths for seizure management in refractory individuals.
Specialized Care in Pediatric Neurology:
Providing specialized treatment for children with epilepsy extends beyond seizure control to address their holistic needs and enhance long-term success. Pediatric neurologists and epileptologists interact closely with pediatricians, neurosurgeons, developmental experts, and educational professionals to build comprehensive treatment plans customized to each child's particular requirements.
Early intervention programs and developmental assessments are key components of juvenile epilepsy management, attempting to reduce the impact of seizures on cognitive and psychosocial development. Furthermore, support services such as speech therapy, occupational therapy, and behavioral therapies play a key role in boosting the quality of life for children with epilepsy and their families.
Transitioning from Pediatric to Adult Care:
As children with epilepsy transition into adolescence and adulthood, they have the issue of negotiating the transfer from pediatric to adult healthcare systems. This transition period involves careful planning and collaboration between pediatric and adult neurology teams to guarantee continuity of care and address the increasing requirements of young patients.
Transition clinics, planned educational programs, and peer support networks assist a smooth transition process, encouraging teenagers with epilepsy to take control of their healthcare journey. Moreover, continued psychosocial support and vocational advice enable young adults with epilepsy to acquire independence and follow their life goals despite the limitations caused by their disease.
Research and Innovation in Pediatric Epilepsy:
Advancements in pediatric neurology and epilepsy research continue to inspire innovation in diagnosis, treatment, and care delivery. Emerging technologies such as wearable seizure detection devices, precision medicine techniques, and novel therapy modalities hold promise for improving outcomes and improved quality of life for children with epilepsy.
Clinical trials and collaborative research projects contribute to the developing knowledge base in juvenile epilepsy, opening the door for tailored and focused therapies. Moreover, advocacy activities and public awareness campaigns play a significant role in destigmatizing epilepsy, promoting early detection, and pushing for equal access to specialized care services.
In summary:
Epilepsy poses particular issues in pediatric neurology, needing a specialized and multidisciplinary approach to management. By understanding the particular features of pediatric epilepsy and embracing novel treatments, healthcare practitioners can optimize results and increase the quality of life for children living with this condition.